The Breast Physiology and the Epidemiology of the Abortion Breast Cancer Link
This past August in Minneapolis, Patrick Carroll, director of the Pension and Population Research Institute of London, presented a paper to the largest gathering of statisticians in North America. He showed that abortion was the best predictor of breast cancer in Britain. Breast cancer is the only cancer in Britain which has its highest incidence and mortality rate among the upper rather than lower social classes. Abortion before a full term pregnancy and late pregnancy were the best explanations for this incidence. He also found that there had been a 70% increase risk of breast cancer between 1971 and 2002 and that for women between 50 and 54 years of age incidence was highly correlated with abortion. In England where the abortion rates are the highest, the incidence of breast cancer is 116 per 100,000, while in Ireland where abortion is rare, the incidence is 97 per 100,000.
Under Ceausescu, during whose 20 year rule abortion was illegal, Romania enjoyed one of the lowest breast cancer rates in Europe. Since abortion was legalized, Romania now has one of the highest breast cancer rates in the world.
These European trends mirror what has occurred in the United States. Over the last 30 years since the 1973 US Supreme Court Roe v. Wade decision legalized abortion in every state, the incidence of breast cancer has risen by 40% while the other major cancers fell or remained the same. Most of this increase occurred in women who were of reproductive age when abortion was legalized. The numbers of abortion performed per year quickly rose from about 60,000 illegal abortions to over 1.5 million performed once abortion was legalized.
Abortion is a causal factor in the development of breast cancer in the same way cigarettes cause lung cancer. Like cigarettes which cause lung cancer to form in 15% of those who smoke, abortion causes breast cancer in about 5% of women who have an abortion. This results in approximately 10,000 cases a year of breast cancer attributable to abortion in the US, approximately the same number caused by the inheritable BRCA gene. The vast majority of smokers never get lung cancer yet we tell the public not to smoke. Women considering abortion need to know about the abortion breast cancer link (ABC link) so that they can give informed consent. Women who have had an abortion need to know they are at higher risk so that they can be screened for breast cancer at an appropriate age.
This article will explain the breast physiology and the epidemiologic criteria supporting the ABC link and briefly comment on two publicized studies refuting it.
Understanding Risk
Many women have been alarmed by the widespread publication of the cumulative life time risk of breast cancer. This is a statistically derived number that assumes all women will live to the age of 82 and not die of other causes before then. For example, in the US in 1975 the risk to develop breast cancer was 1 in 12 women. In 2004 that risk increased to 1 in 7, reflecting the increase in incidence of breast cancer over the last 30 years. However, it does not mean that if there are seven women in a room one of them will now develop breast cancer. If a woman in the US has no risk factors for breast cancer, and very few women do, her risk of developing breast cancer is 3.3%.1
I Three Major Influences on Breast Cancer Risk
The risk for development of breast cancer can be understood by considering three major influences: genetic factors, lifetime exposure to estrogen and breast lobule maturation. Genetic factors can include inheritable mutated genes as well as physical or chemical carcinogens. Well documented breast physiology in relation to estrogen and lobule maturation fully supports the association of induced abortion and breast cancer risk.
1. Genetic Factors
While it is true the root cause of all cancers are damaged genes, when considering breast cancer risk it is useful to realize that only 8 to 10% of all breast cancers occur because women inherited a faulty gene from one of their parents such as the BRCA genes. There can also be direct DNA damage caused by large doses of radiation to the breast such as when women are treated for Hodgkin’s disease in the chest with radiation. These account, however, for only a few percent of cancer cases. Benzopyrenes in cigarette smoke can also damage breast DNA.
Therefore, lifetime exposure to estrogen and breast lobule maturation account for the
approximate 90% of the other cases of breast cancer. There is also the interaction of these two factors in regards to the timing of these exposures that impact risk. For example, exposure to radiation damages breast tissue most when the cells are actively developing and dividing as when the breast is growing during puberty. The atomic bomb radiation in Hiroshima caused breast cancers to form in teenagers that were exposed and did not affect postmenopausal women. Benzopyrenes in cigarette smoke increase breast cancer risk in teenagers who have not had children by as much as 600%.2 Postmenopausal women who have had children do not have this increase in risk.
2. Lifetime Exposure to Estrogen
Estrogen is the major female hormone which makes women womanly. Without estrogen women would not develop breasts or be able to bear children. It is difficult to grasp why such a beneficent hormone could also cause breast cancer. Yet one only has to remember that some of the most effective and used breast cancer treatments available are drugs which block the effect of estrogen or keep it from forming in the patient in order to understand the large impact estrogen exposure has on the risk of developing breast cancer. The class of anti-cancer drugs known as SERMs alter the effect of estrogen on breast cells. For example, tamoxifen (Nolvadex®), a drug used both to treat breast cancer and prevent it, blocks estrogen receptors. Another class of drugs such as anastrozole (Arimidex®) blocks an enzyme aromatase from converting another hormone into estrogen. Before such drugs were available, breast cancer was treated by removing the patient’s ovaries to decrease the estrogen in her body.
DES, diethyl stilbesterol, a potent synthetic estrogen used to prevent miscarriages also increased the risk of breast cancer in the mother and the female child exposed in utero. In order to understand why lifetime exposure to estrogen increases breast cancer risk, it is necessary to understand its role as a mitogen and genotoxin.
Estrogen as a Mitogen
Estrogen in the presence of progesterone causes breast cells to undergo mitosis, i. e. multiply through division. Once a breast cell duplicates its DNA (long strands of genes in the nucleus of the cell) it will divide into two cells. While the DNA is duplicated, copying errors and translocations can occur resulting in cells with abnormal DNA called mutations. If a mutation is severe enough or if multiple mutations occur, a cancer cell may form.
Towards the end of a woman’s menstrual cycle, estrogen and progesterone levels are elevated causing milk duct cells to undergo mitosis. These facts account for many risk factors of breast cancer that can be summed up by noting that the more menstrual cycles a woman has in her lifetime the higher her risk for breast cancer. For example, early menarche (age at 1st menstruation) and late menopause result in more menstrual cycles and are factors which increase breast cancer risk. Late menarche and early menopause result in fewer cycles and decrease risk of breast cancer. Irregular cycles in the first few years after menarche result in lower breast cancer risk (fewer cycles and fewer ovulations). Teenagers may be treated with birth control pills to regulate their cycles, thereby increasing breast cancer risk.
Estrogen as a Carcinogen
Estrogen also causes breast cancer by directly acting as a carcinogen, i. e. by directly damaging DNA. There are metabolites of estrogen which the body makes in the course of breaking down the hormone and eliminating its effect. Hormone levels in the body are tightly regulated on a daily as well as monthly cycle basis. One such metabolite of estrogen is catechol estrogen quinone (CE quinone). CE quinone directly damages DNA by pulling purine bases, components of DNA, out of the strands. Women with breast cancer have higher levels of CE quinone in their blood than women without breast cancer.3
In premenopausal women the ovaries are the primary natural source of estrogen. By removing the ovaries, a woman will have a lower risk of breast cancer. This may happen if a woman has her ovaries removed because of disease. There is also a peak of estrogen during the menstrual cycle that causes ovulation. When a woman is under stress, for example during marathon training or by extreme weight loss, she may not ovulate or miss her cycles altogether reducing her breast cancer risk. During breast feeding a woman may also miss ovulation or cycles reducing breast cancer risk. The primary source of natural post menopausal estrogen is adipose (fat) tissue. The aromatase enzyme system in adipose cells causes estrogen to be formed from another hormone, androstendione. Therefore postmenopausal obesity also increases risk for breast cancer.
Estrogen can also come from sources outside the body, usually as drugs and sometimes as residues found in foods. Worldwide, about 10% of all women of reproductive age presently use combined hormonal contraceptives. In all, there are more than 100 million women who take combined oral contraceptives. The rates vary from 6% in less- developed countries to 16% in more well-developed countries. In the US about 75% of women have taken hormonal birth control in their lives. As explained in a later section on breast lobule maturity, this is especially potent in forming breast cancers when taken by teens or women without children. Most birth control pills contain estrogen and progesterone at high enough levels to largely suppress ovulation. One study showed teenagers who take birth control pills before a pregnancy have a 1000% increase risk of breast cancer.4 Injectable and implantable progestin-only drugs increase risk as would the hormones taken transdermally with a patch. Hormone replacement therapy also increases breast cancer risk commensurate with the length of time it was taken. In Puerto Rico, estrogen residues found in chicken meat were responsible for early menarche in teens increasing their breast cancer risk.
Recent Acknowledgement of Carcinogenic Effects of Estrogen
In August 2005, Lancet Oncology reported that as a result of this past June’s meeting of the International Agency for Research on Cancer in Lyon, France, the World Health Organization recognized that estrogen and progesterone taken in combination, resulted in increased risk of breast as well as cervical and liver cancers.5 Estrogen has been listed as a carcinogen by the National Toxicology Advisory Panel of the US National Cancer Institute since 2000 precisely because they felt women weren’t being apprised of their risk of breast cancer sufficiently when hormone replacement therapy and birth control pills were prescribed. By scientists demonstrating that even breast cells that do not have estrogen receptors in them will become cancerous when exposed to estrogen confirms that estrogen is a direct carcinogen.6 The estrogen receptors do not need to be stimulated for mitosis in order to initiate a cancer. Estrogen can directly initiate cancer cells to form. The age specific incidence curve for breast cancer underscores this fact as the incidence of breast cancer does not start to increase until after puberty and rises sharply at the point when initiated cancers become clinically detectable, about 10 years after menarche. The incidence does not lessen until after menopause.
This is why estrogen-containing drugs should not be used for most of their widely applied usages when there are other equally effective methods for treatment. The drugs Fosamax® (alendronate sodium) and Actonel® (risendronate sodium) can be used for osteoporosis. Heart attacks and strokes as well as blood clots in veins and lungs are increased by hormonal treatments. Acne can be treated with antibiotics. Irregular cycles in teens are normal and reduce cancer risk. Painful menstrual cramps can be treated with pain relieving antiinflammatory drugs. Fertility can be controlled with natural methods such as tracking fertile days and abstinence or non hormonal barrier methods. Cancer causing drugs should be used only when no other methods or treatments are available.
3. Breast Lobule Maturation
The breast is the only organ that is not fully formed at birth. It does not start to fully develop until puberty when estrogen levels start to rise and the breast enlarges. However, it does not fully mature until the end of a full term pregnancy when it is capable of producing milk for a newborn.7
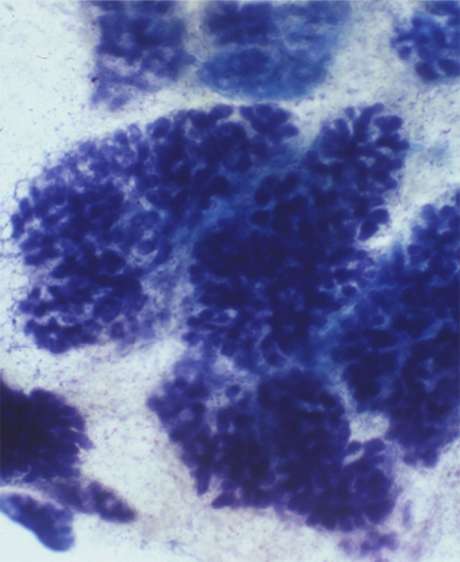
To the eye, the breast merely enlarges during pregnancy. Microscopically, and more importantly, the breast actually changes its microscopic structure into cancer resistant type 3 lobules. This is why having a full term pregnancy reduces a woman’s risk of breast cancer and the earlier she does this in her reproductive life, the lower her risk of breast cancer. When a female child is born she only has a few rudimentary alveolar buds. At the end of puberty, over 70% of her breast tissue consists of type 1 lobules. These are units of breast tissue consisting of milk glands and a duct which are immature and incapable of producing milk. They are also the place where ductal breast cancers start. Ductal breast cancers account for over 80% of all human breast cancers. Not only do they look different anatomically, but they also act different metabolically. For instance, they replicate their DNA faster than mature type 3 lobules. This results in more copying errors and mutations than in type 3 lobules. There is also a shorter time for the cell to repair the errors. After undergoing a full term pregnancy, only a small percentage of the type 1 lobules remain and over 70% of the breast tissue is now the cancer resistant type 3 lobules. This is why a full term pregnancy reduces breast cancer risk. It is also why the sooner a woman has a full term pregnancy the lower her risk of breast cancer. After a full term pregnancy, further exposure to estrogen during her monthly cycles does not as adversely effect her breasts as would be the case if her breasts were still mostly composed of cancer sensitive type 1 lobules. If a woman has menarche at age 10 and doesn’t have a full term pregnancy until she is 30, she has had 20 years of estrogen exposure by her cancer sensitive type 1 lobules. If she has a full term pregnancy at age 20, there will have been half the risk exposure and less cancer risk. In fact, compared to a woman who has her first full term pregnancy at age 30, an 18 year old who has a full term pregnancy has a 75% reduction in breast cancer risk.
If a woman remains childless, for her entire reproductive life her sensitive type 1 and 2 lobules are exposed to elevated levels of carcinogens for over 30 years and her risk of breast cancer is greatly increased.
The effect of pregnancy hormones on the breast is different at different times during the pregnancy. During the first two trimesters in the presence of rapidly rising levels of estrogen, the breast merely enlarges by increasing the numbers of type 1 and 2 cancer vulnerable lobules. This is why premature deliveries before 32 weeks of pregnancy increases breast cancer risk. When the pregnancy ends at premature delivery, the breast has not matured into mostly type 3 lobules resistant to cancer, but is now different than the pre-pregnancy state. There are now more type 1 lobules in the breast and more places with breast cancer to start. This assumes that the hormonal status of the pregnancy is normal and resulted in a pregnancy that lasted up to 7 months.
a) Spontaneous Abortions
However, some pregnancies end prematurely through spontaneous abortion (also known as miscarriage). Most of these spontaneous abortions occur in pregnancies with low hormonal levels. Women will often report not having realized they were pregnant when they miscarried. They had not experienced the earliest signs of pregnancy such as sore and tender breasts or nausea as their hormonal levels were not elevated as in a normal pregnancy. Estrogen level will rise even before implantation and increase 2000% by the end of the first trimester. Doctors will often measure estrogen levels when attempting to predict when bleeding during pregnancy will result in spontaneous abortion. If levels are below normal, the pregnancy is not healthy and the mother will miscarry.
b) Induced Abortions
These situations are very different from those that occur in induced abortions. Most of these occur in normal pregnancies. Studies have shown that the longer a pregnancy exists before an abortion, the higher the risk of breast cancer. This is due to the same mechanism why premature births increase breast cancer risk. After an induced abortion, the mother is left with more type 1 and 2 lobules where cancers start than before she was pregnant. This causes her to be at increased risk for breast cancer. This is the basis for the independent risk of abortion and breast cancer.
There are also secondary reasons why induced abortion increases breast cancer risk. A woman who is pregnant and gets an abortion loses the protection against breast cancer a full term pregnancy would have afforded her. She is exposed to very high levels of the mitogen and genotoxin estrogen even in early abortions. Abortions also increase the incidence of premature deliveries of subsequent pregnancies which in themselves increase breast cancer risk.
Summary
Abortion increases breast cancer risk through multiple mechanisms. Pregnancy exposes the woman to high levels of estrogen acting as a mitogen and genotoxin and induced abortion then leaves her breast with more places for breast cancers to start. She has a higher risk of subsequent premature deliveries which then increase her risk further.
II Epidemiologic Support for the ABC Link
Epidemiology is defined as the study of disease trends in large populations. It cannot by itself be the method to discover the cause of diseases. Scientists usually do that with experiments and case studies of patients. Epidemiologic studies give scientists a place to look for corroboration. However, if epidemiologic studies are done and they meet certain criteria as a whole, the case for a causal relationship can be made.
Before any statements may be made, that a factor is a real cause of a disease and not just merely associated with it, strict criteria must be met. Just because a study shows a positive association of a factor with a disease, it doesn’t mean that factor is the cause.
For example, large, statistically significant and reproducible studies might show that people who carry matches in their pockets have a higher risk of lung cancer. We know now that the cigarettes they light cause the lung cancer. Without the additional criteria of a plausible biologic theory of how the matches cause lung cancer, these studies, no matter how many are done, show only a positive association between matches and lung cancer.
Knowing that matches were associated might lead scientists to investigate how the matches were used and discover the true cause of lung cancer.
1 Nine Criteria illustrating the causal risk of Abortion and Breast Cancer
Epidemiologic studies done concerning the ABC link show that they meet nine criteria for abortion becoming a causal factor for developing breast cancer.
Criterion 1: Timing
The exposure to the risk must occur before the disease is detected, i.e. the abortion must occur before the breast cancers form. This may seem so obvious that it need not be mentioned. However, a well known study, the 1997 Melbye study violated this rule when it collected breast cancer cases from a registry starting in 1968 and abortions starting in 1973. Those cases of cancer from 1968 to 1972 should not have been included in the study.8
Criterion 2: The preponderance of studies shows a positive association between abortion and breast cancer.
One or two studies can never be thought to prove a causal link. Out of 40 world wide studies done to date, 27 show a positive association.
Criterion 3: Statistically significant studies
Scientists require 95% certainty that the study results were not obtained by chance alone. There are 17 statistically significant studies which show the ABC Link.
Criterion 4: Studies show a large relative risk, greater than 3.0
If there is only a 10% increase in risk, it is difficult to say the risk is causal. There are subsets of women that show a greater than 200% increase risk in breast cancer with abortion.
Criterion 5: The dose effect
Based on biologic mechanisms, the more one is exposed to the risk, the higher the risk to develop the disease. For example, the more cigarettes one smokes, the higher the risk of lung cancer. The longer one is pregnant before an abortion, the higher is the risk of breast cancer. This is because the woman is left with more type 1 and 2 lobules where breast cancers start than at the time of conception.
Criterion 6: Biologic plausibility
The biologic mechanism that explains the reason for the risk association must be biologically plausible. The physiology of the breast cancer link with abortion has been thoroughly explained in a previous section. Elevated levels of estrogen during pregnancy leave the breast with increased numbers of type 1 and 2 lobules where breast cancers arise and there is no benefit of a full term pregnancy maturing the breast with predominantly type 3 lobules which are cancer resistant.
Criterion 7: Experimental studies
In 1980, Russo and Russo studied the effect of abortion on rats compared to rats that had a full term pregnancy. The aborted rats developed breast cancers at a much higher rate when given the carcinogen DMBA than virgin or rats that had had a full term pregnancy.9
Criterion 8: Analogy
Similar exposures should result in similar effects. Premature deliveries before 32 weeks also double breast cancer risk because the breasts are left with more lobules where breast cancers can start.10 An abortion can be thought of as premature delivery by an abortionist.
Criterion 9: Coherence
The association of breast cancer and abortion should be compatible with the known natural history and biology of breast cancer. It takes an average of 8 to 10 years for one breast cancer cell to keep doubling so that it forms a tumor of clinically detectable size, about 1 centimeter. The time periods in studies show the increase in breast cancers occur in the time frame appropriate for the development of breast cancer, i. e. at least 8 to 10 years after exposure.
2 Recent Epidemiological Studies and the Abortion Breast Cancer Link
In 1996, in the British Journal of Epidemiology and Community Health, Dr. Joel Brind and a group of US scientists published a quantitative meta-analysis of all the studies done up until that time which differentiated induced and spontaneous abortions. He found there was an overall 30% increase risk of breast cancer in women who had an abortion. This created such a furor that the journal’s editor, Stuart Donan, felt he had to write an editorial in the following month’s edition stating that although he was himself “pro-choice”, he felt one must also be “pro-information”.
Since that 1996 meta-analysis, there have been some recent studies that do not support the abortion breast cancer link. The most recently well publicized study was published March 2004 in the journal Lancet.11 One of the authors quoted in a major Atlanta paper said, “Scientifically, this is really a full analysis of the current data.”12 Nothing could be further from the scientific truth. Out of many flaws in the study, three of them will be addressed here. (1) Selection bias occurred when 14 of 41 previously published were excluded for non-scientific reasons or simply not acknowledged to exist. The authors excluded 10 of 16 statistically significant studies linking abortion and breast cancer. If these 14 studies were combined they would show an 80% increase in breast cancer risk. (2) The authors also made an assumption of “recall bias” because their own study revealed an 11% increase in risk when retrospective studies were used. Recall bias assumes that women with breast cancer will more likely admit an abortion history and women without cancer will more likely lie. Recall bias is an hypothesis which has never been proven to show a statistically significant difference in these groups even when explicitly tested. (3) An inappropriate comparison group was chosen. The authors compared apples and oranges when the effects of having had a pregnancy that ended in abortion were compared with the effect of “not having had that pregnancy.” Once a woman has begun a healthy pregnancy, however long, her breasts are different from before that pregnancy started. Just as the effect of hormone replacement for postmenopausal women is studied in relation to other postmenopausal women who have no exposure to hormones, pregnant women who undergo abortion need to be compared to pregnant women who do not undergo induced abortion. Pregnancy forever alters the breast and physiologically these women are as different as pre- and postmenopausal women.
Another study published in 1997 misclassified 60,000 women who had legal abortions as not having had abortions because the authors used abortion registries starting in 1973 instead of 1940.13 Yet even with this and other major flaws, the study showed a statistically significant increase in risk in 2nd trimester abortions. This fact was not mentioned in the conclusion of the paper which stated that there was no link between abortion and breast cancer.
Conclusion
There has been created a need in society for “safe and legal” abortions as recourse when contraception fails. Even the US Supreme Court has used the argument that the public good demands abortion as a back up for failed contraception. If abortion is shown to be unsafe and a cause of human cancer that has hurt women, would constraints on reproductive rights not follow? This fear has polluted the normal scientific discourse that is needed. Our human biology will not allow us to avoid the obvious. Breast cancer and abortion are linked. Women know this on many levels. Rampant breast cancer seen in ever younger women will not allow this issue to be suppressed no matter how big the business of abortion providers. Breast cancer organizations should take the lead in informing women about the risks not only of abortion but also of the carcinogenic effect of estrogen-progestin combination drugs.
References
- Newell G. R., Vogel V. G., Personal risk factors: What do they mean?, Cancer (1988); 62: 1695
- Band P. R., Le N. D., Deschamps M., Carcinogenic and endocrine disrupting effects of cigarette smoke and risk of breast cancer, Lancet (2002);360: 1044
- Rogan E. G. et al., Relative imbalances in estrogen metabolism and conjugation in breast tissue of women with carcinoma: potential biomarkers of susceptibility to cancer, Carcinogenesis (2003); 24(4): 697-702
- Olsson H., Landin-Olsson M. Muller T. R., Oral contraceptive use and breast cancer in young women in Sweden (Letter), Lancet (1985); 1: 748-749
- Cogliano V. et al., Carcinogenicity of combined oestrogen-progestagen contraceptives and menopausal treatment, Lancet Oncology (2005); 56: 553-553
- Miller K., Estrogen and DNA Damage: The Silent Source of Breast Cancer?, J Natl Cancer Inst (2003); 95(2): 100-102
- Russo J., Russo I. J., Influence of age and parity on the deve-lopment of the human breast, Breast Cancer Res Treat (1992); 23: 211-218
- Melbye M. et al., Induced Abortion and the Risk of Breast Cancer, N Engl J Med (1997); 336: 81-85
- Russo J., Russo I. H., Susceptibility of the Mammary Gland to Carcinogenesis, Am J Pathol (1980); 100: 497-512
- Melbye M. et al., Pre-term Delivery and Risk of Breast Cancer, Br J Cancer (1999); 80: 609
- Beral V. et al., Breast Cancer and Abortion:Collaborative Reanalysis of Data from 53 Epidemiological Studies, Including 83,000 Women with Breast Cancer from 16 Countries, Lancet (20049, 363: 1007-1016
- Wahlberg D., Study: Breast Cancer Not Tied To Abortion; Group Backs Up Institute’s Earlier Findings, Atlanta Journal Constitution (GA), March 26, 2004, A9
- Melbye M. et al., Induced Abortion and the Risk of Breast Cancer, N Engl J Med (1997); 336: 81-85

Dr. Angela Lanfranchi MD, FACS
Breast Cancer Prevention Institute
9 Vassar Street, Poughkeepsie, New York
12601, USA
angelabcpi(at)yahoo.com